Meningoencephalitis
Postnatal
Meningoencephalitis
Meningoencephalitis in infants
often has a worse outcome than in older patients. Infectious diseases of the
brain often lead to the death of the patient or to severe complications.
complications
In more than one half of the
patients, meningoencephalitis is complicated by
1.
postmeningitic hydrocephalus
2.
subdural effusions
3.
cerebral infarction
4.
ventriculitis
5.
brain abscess
6.
cerebral vasculopathy .
Prenatal and neonatal infections
are complicated by postmeningitic hydrocephalus in more than 2/3 of the cases.
Infectious diseases with
gram-negative bacteria often lead to prognostic unfavourable ventriculitis. Rare
complications in this age group are subdural effusions, porencephalic cysts and
brain abscesses . Beyond the neonatal period complications occur much rarer.
Meningoencephalitis in later infancy is complicated in only one third of the cases
by postmeningitic hydrocephalus and postinfectious subdural effusions in 20 %
of the cases .
Features
1.
Meningoencephalitis is characterised by :
2.
Arachnoiditis
3.
Ventriculitis
4.
Vasculitis
5.
Brain oedema pathologically .
Especially in the acute phase of the disease,
vasculitis and the developing brain oedema may influence blood flow. Later on,
brain perfusion may be influenced by progressive ventricular dilatation as well
as by subdural effusions .
In the acute phase the disease is complicated by vasculitis and brain
oedema which may influence the flow in the intracranial arteries. Vasculitis is
nearly always found in bacterial meningitis . Pathologically phlebitis can be
differentiated from arteritis. Infectious infiltrates of the adventitia of the
arteries may lead to obstruction of the vessels. Complete arterial occlusion
however is very rare. Infectious infiltrates within the veins can be found more
frequently. Phlebitis is often complicated by thrombosis or complete occlusion.
Vasculitis can already be found in the first days of the disease. It is however
most prominent in the 2nd or 3rd week of the disease .
2D Image
2D images have to distinguish
between acute and chronic changes. In the acute phase, signs of bacterial infection,
such as pus or brain oedema, have to be ruled out. Later images show postinfectious
hydrocephalus, subdural effusions, ventriculitis and abscess formation.
2D Images
in the Acute Phase
Besides vasculitis a more or
less severe brain oedema may be found in association with meningoencephalitis.
Oedema may be so severe that the
ventricular system is slit-like or can no longer be shown in the individual
case. Oedema is caused by increased permeability of the vessels caused by
vasculitis (vascular oedema) and by cell death (cytotoxic oedema) caused by bacterial
toxins .
2D images show
1.
Increased echogenicity of the brain tissue and the subdural space . Increased echogenicity of the brain can best be shown
on midline sections .
2.
Focal increased echogenicity: can be found within the brain tissue . It may be caused by focal
brain oedema, brain abscesses or vascular occlusion. The various Doppler
techniques can help by the differential diagnosis .
2D in
Chronic Changes
Postinfectious alterations are :
1.
postmeningitic hydrocephalus
2.
subdural effusions
3.
porencephalic cysts
4.
abscess formation
5.
ventriculitis.
They usually occur with a delay
of several days to some weeks. Therefore, serial sonographic investigations
have to be performed .
postmeningitic
hydrocephalus
As mentioned earlier postmeningitic hydrocephalus occurs very often in neonatal meningitis . The shape
of the ventricular dilatation does not differ from posthaemorrhagic hydrocephalus.
postmeningitic
subdural effusion
The second complication is postmeningitic subdural effusion. Imaging techniques are not different from other
dilatations of the subdural or subarachnoid space. Subdural empyema is characterized
by hyperechoic fluid collections over the convexity of the brain, hyperechoic
fibrinous strands and thick, hyperechoic inner membranes in most patients .
Ventriculitis
is characterized by increased echogenicity
within the dilated ventricles . The inner surface of the dilated ventricles appears
echogenic due to ependymitis. Additionally fibrin fibres may transverse the
ventricular space .
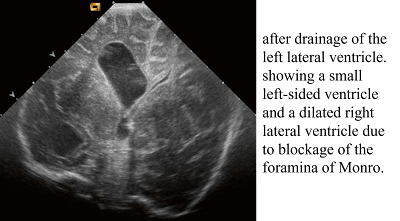
Unfortunately postmeningitic hydrocephalus
often develops which has to be treated by a ventriculoperitoneal shunt. A
severe complication after ventriculitis is the development of a compartment hydrocephalus.
Compartment hydrocephalus
are characterized by missing communication of
the different parts of the ventricular system with each other. The
cerebrospinal fluid is produced by the choroid plexus of the lateral
ventricles, the third and the fourth ventricles. If the different parts of the
ventricular system do not communicate with each other, a single ventricular
catheter will not be able to drain the complete ventricular system. A
ventricular catheter, placed in one dilated lateral ventricle, will not be able
to drain the whole ventricular system if the foramina of Monro or the cerebral
aqueduct are obstructed. Therefore, different draining catheters have to be
placed within the not communicating parts of the ventricular system . Another
possibility is endoscopic creation of new communications between the different
ventricles (e.g. third ventriculostomy or septostomy).
Postmeningitic abscesses
may occur after infections with
staphylococci and gram-negative bacteria and after fungal infections. They
appear as areas of increased echogenicity . After several days they may develop
a liquid centre . If multiple small echogenic foci scattered all over the brain
are found, fungal infection is very probable .
Doppler
Sonography
Colour
Doppler
If colour or power Doppler
sonograms are performed, increased vascularity can be found. The increased
vascularity is typical for meningoencephalitis . Sometimes focal increased
echogenicity can be found on 2D images . With the help of colour or power
Doppler, differentiation between arterial or venous occlusion and infectious infiltrates
can be performed . Infectious infiltrates show increased vascularity, whereas
arterial occlusion or venous thrombosis is free of vessels .
Spectral
Doppler
Doppler sonographic flow
measurements in intracranial arteries of patients with meningoencephalitis showed
an increase of all flow velocities. The mean flow velocities in patients with
bacterial meningitis were significantly increased . The mean cerebral flow
velocities were significantly higher in patients with neurological sequelae .
As peak systolic, end-systolic
and end-diastolic flow velocities are simultaneously increased, the resistive
index does not significantly differ from a control collective of healthy infants
. The increase of the flow velocities is probably caused by the narrowing of
the arteries caused by associated brain oedema and vasculitis.
According to the continuity
equation of Bernoulli, inflow in narrow vessels
equals outflow. Within physiologic limits a decrease of the vessel diameter leads
to an increase of the flow velocities. A further decrease of the diameter of
the arteries may theoretically lead to a decrease of the diastolic flow
velocities while systolic flow is still increased. A retrograde diastolic flow
would be typical for a marked increase of the intracranial pressure over the
diastolic blood pressure. Retrograde diastolic flow could never be found in our
patients with meningoencephalitis. If flow measurements are performed
simultaneously in the extracerebral and intracerebral section of the internal
carotid artery, the flow velocities increase in the intracranial part of the artery
due to brain oedema . According to our experience, this is the first and most
sensitive sign of increasing intracranial pressure.
ventriculitis
If colour Doppler shows flow of
the cerebrospinal fluid within the sylviduct and the foramina of Monro, this is
a sensitive sign of associated ventriculitis. In these cases small particles within
the cerebrospinal fluid reflect the ultrasound beam. These reflecting particles
are leucocytes indicative of associated ventriculitis. In these cases
cerebrospinal fluid flow can be
shown by colour Doppler and spectral Doppler within the physiologic constrictions
of the ventricular system.
The flow is either :
1.
ventriculopedal
(e.g. from the fourth to the third ventricle)
2.
ventriculofugal
(e.g. from the third to the fourth ventricle) .
Colour Doppler shows
ventriculofugal flow blue and ventriculopedal flow red . Pulsed Doppler reveals
ventriculofugal flow beneath the baseline, whereas ventriculopedal flow is
displayed above the baseline . Ventriculopedal flow is caused by respiratory
movements and by moderate compression of the abdominal wall.
meningitis complicated by
ventriculitis
Doppler sonography can be used
for the diagnosis of meningitis complicated by ventriculitis. In the case of
postmeningitic hydrocephalus associated with ventriculitis, colour Doppler can show
if the aqueduct is open or if stenosis or occlusion has occurred.
Prenatal
Infections of the Brain
Prenatal infections that may
affect the developing brain are described by the TORCH infections (toxoplasmosis,
syphilis, HIV, rubella, cytomegalovirus and herpes simplex). Depending on the time
of infection, they may cause :
·
Microcephaly
·
disturbances in neuronal migration
·
cerebellar hypoplasia
·
haemorrhagic or leucomalacic lesions
·
periventricular and/or cortical calcifications
·
subependymal cysts
·
vasculopathy of the lenticulostriatic vessels
Sonographically vasculopathies
appear as linear or punctate echodensities within the basal ganglia that often
are candlestick shaped . Colour Doppler confirms the vascular nature of the echodense
stripes . Within the walls of the lenticulostriatic arteries and veins, basophilic
material as well as mineralisation and hypercellularity was found .
Vasculopathy of the
lenticulostriatic arteries
is not specific for a specific prenatal
infection (e.g. cytomegalovirus). Other prenatal infections of the brain such
as HIV, rubella, syphilis infections, etc. may cause vasculopathy of the basal ganglia
too . However, vasculopathy of the basal ganglia is also not specific for
prenatal infections of the
brain . It can additionally be
found in chromosome anomalies (e.g. trisomy 13 and 18), dysmorphic syndromes,
lysosomal disorders (sialidosis), inborn errors of metabolism (glutaracidemia
type 1), asphyxia and other
diseases . In any patient with
stripe-like or punctate echogenicities of the basal ganglia, prenatal infections, caused by TORCH infections, and inborn errors of
metabolism have to be ruled out.
If these infants do not look syndromic and
have no signs of inborn errors of metabolism and TORCH infections have been
excluded, possibly no serious disease is present.